This effort reflects a philosophical shift toward fostering wellness, rather than just treating illness, as an essential element to help reduce health care costs and expand access to primary care. This requires an emphasis on understanding and addressing the social determinants of health, encouraging disease and injury prevention, and creating a culture of wellness. It also requires understanding that nurses today are being educated for a far more comprehensive role in delivering health care.
Elevating the role of nursing and nursing education will ultimately mean better access to care — especially primary care — particularly in states such as Washington that have substantial rural and underserved populations. Nurses whose education has given them a doctorate or advanced practice status provide excellent primary care at relatively low cost compared with physicians, and they are more likely to serve in traditionally underserved areas.
In 2009, the Robert Wood Johnson Foundation partnered with the Institute of Medicine (now the National Academy of Medicine) to explore the role of nursing and nursing education. The result, published in 2011, was The Future of Nursing: Leading Change, Advancing Health, a comprehensive report that created a vision for nursing in 2020. The report noted that both economics and logistics have been factors in causing physicians to cluster in urban areas, leaving gaping geographic holes in what should be a uniform net of primary care providers.
“By virtue of their regular, close proximity to patients and their scientific understanding of care processes across the continuum of care, nurses have a considerable opportunity to act as full partners with other health professionals and to lead in the improvement and redesign of the health care system and its practice environment,” the report concluded.
The University of Washington School of Nursing and other leading schools throughout the nation responded by significantly expanding goals, facilities and curricula in order to encompass the report’s recommendations, and expanded its capability to educate more nurses to a higher level of practice sophistication. Today, more than 28,000 nurses nationwide who are employed hold doctoral degrees — a number that more than doubled between 2011 and 2017.
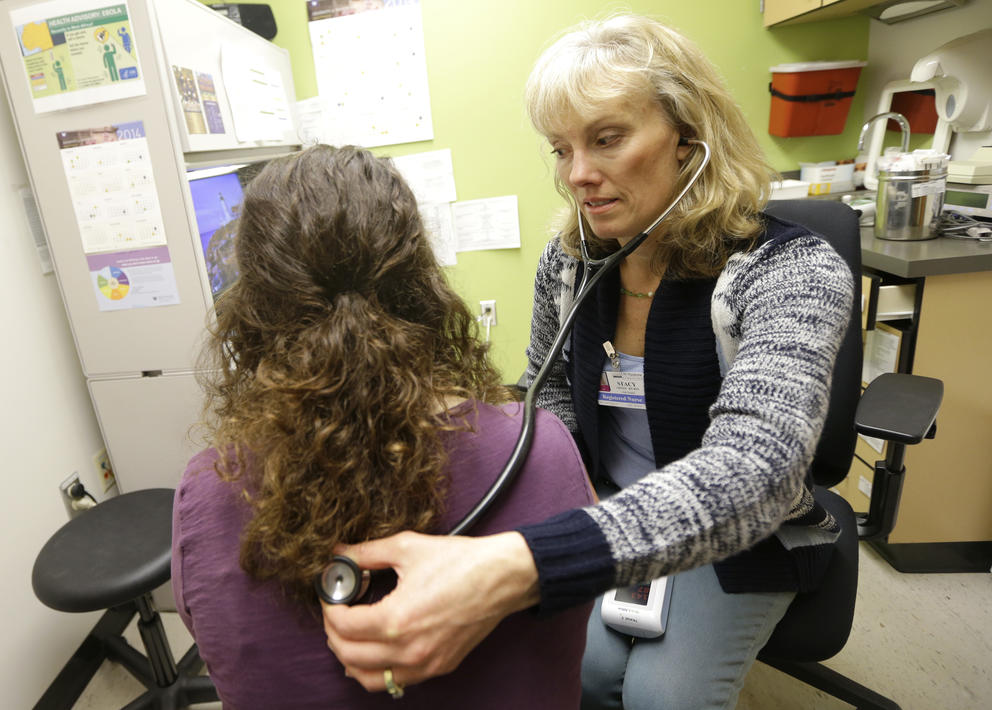
Nurses are the backbone of care in every hospital, but we need greater public awareness of the full range of capabilities for which nurses are being educated today. An ever-increasing number of nurses have doctor of nursing practice (DNP) degrees. They provide independent, economical primary care that studies have consistently found to be without compromise, and they often do so while serving populations in rural areas, on Indian reservations, and in underserved urban communities. For example, the Community Health Association of Spokane (CHAS) established a very busy Nurse Practitioner Residency Clinic to provide access to primary care in an underserved area of Spokane. The success of this clinic encouraged CHAS to seek expansion into very rural areas in southeast Washington. And the International Community Health Services clinic in the Seattle Chinatown-International District established a highly successful nurse practitioner residency program that has attracted and retained newly graduated nurse practitioners. This has allowed the organization to expand its clinics to serve Shoreline and Holly Park, two underserved urban areas
Many other nurses have advanced practice degrees and certifications that enable them to serve as nurse practitioners, nurse anesthetists, nurse midwives and clinical nurse specialists. Nurses holding Ph.D. degrees are active researchers in academic and corporate settings, advancing medical knowledge about myriad diseases and conditions, and providing the foundation for enhanced diagnostic and treatment options across the entire lifespan. In Washington state, nurses are educated, licensed and ready to fulfill a far more robust role in the health care system than they could a decade ago.
Because educational and regulatory change takes time, we as a profession are once again looking ahead and asking how best to prepare for the future and the role of nurses. The National Academy of Medicine has formed a Committee on the Future of Nursing 2020-2030. Its task is to “extend the vision for the nursing profession into 2030 and to chart a path for the nursing profession to help our nation create a culture of health, reduce health disparities, and improve the health and well-being of the U.S. population in the 21st century.”
The committee held a public listening session in March (materials from that session are available online). The committee will hold a series of town hall meetings for health care professionals this year in Chicago, Philadelphia and at the University of Washington School of Nursing in Seattle. The public can register to attend or watch the Seattle event or any of the three meetings online.
These discussions are about your health care future. Watch, listen and let your opinion be known. This is your opportunity to help shape the future of our health care system. Legislators, policy makers and members of the executive branch need to know what the public thinks about the future of health care and the role of nursing in creating and implementing that future.
Transforming the U.S. health care system is an enormous and complex job. It is vital that everyone has a seat at the table as possibilities are discussed, implementation is planned, and funding is sourced. Public opinion can create legislative momentum and direct the necessary resources to create a more effective, more efficient and more equitably accessible health care system for everyone.